Introduction
Physiotherapy in Toronto for Pediatric Issues
Welcome to In Balance Physiotherapy’s Guide to Perthes Disease of the Hip.
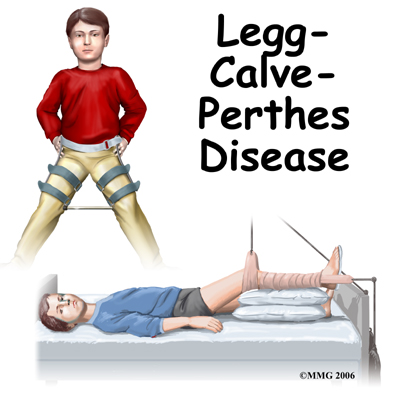
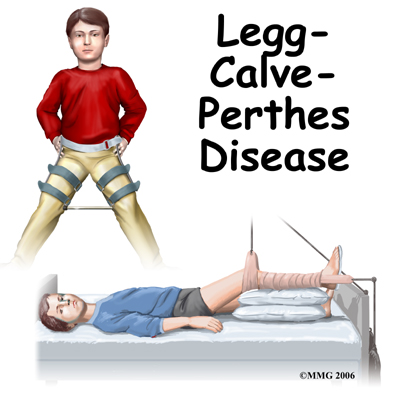 Perthes disease is a condition that affects the hip in children between the ages of four and eight. The condition is also referred to as Legg-Calve-Perthes disease in honor of the three physicians who each separately described the disease. In this condition, the blood supply to the growth center of the hip (the capital femoral epiphysis) is disturbed, causing the bone in this area to die. The blood supply eventually returns, and the bone heals. How the bone heals determines what problems the condition will cause in later life. Perthes disease may affect both hips. In fact, 10 to 12 percent of the time the condition is bilateral (meaning that it affects both hips). This condition can lead to serious problems in the hip joint later in life.
Perthes disease is a condition that affects the hip in children between the ages of four and eight. The condition is also referred to as Legg-Calve-Perthes disease in honor of the three physicians who each separately described the disease. In this condition, the blood supply to the growth center of the hip (the capital femoral epiphysis) is disturbed, causing the bone in this area to die. The blood supply eventually returns, and the bone heals. How the bone heals determines what problems the condition will cause in later life. Perthes disease may affect both hips. In fact, 10 to 12 percent of the time the condition is bilateral (meaning that it affects both hips). This condition can lead to serious problems in the hip joint later in life.
This guide will help you understand:
- what part of the hip is involved
- what causes the condition
- what treatment options are available
- what In Balance Physiotherapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Pediatrics|limit:15|heading:Hear from some of our *Pediatrics* patients#
Anatomy
What part of the hip is affected?
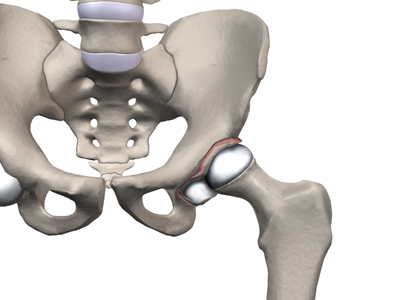
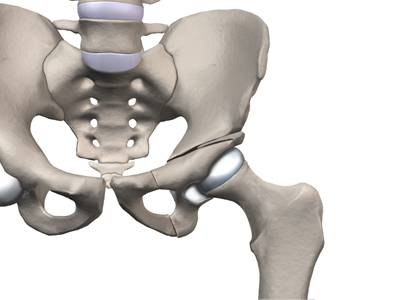
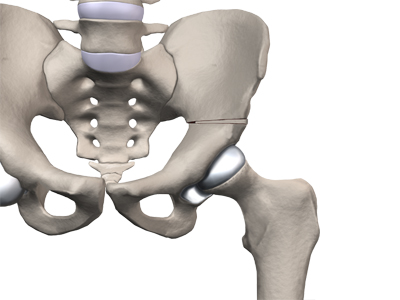
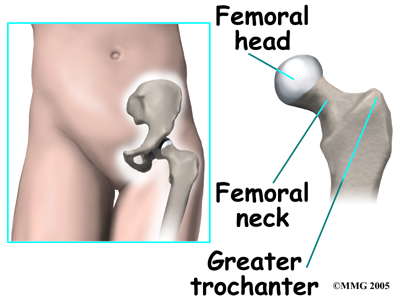
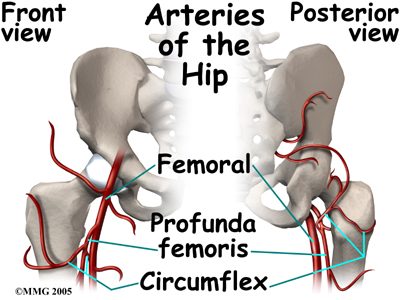
The hip joint is where the thighbone (femur) connects to the pelvis. The joint is made up of two parts. The upper end of the femur is shaped like a ball. It is called the femoral head. The femoral head fits into a socket in the pelvis called the acetabulum. This ball and socket joint is what allows us to move our leg in many directions in relation to our body.
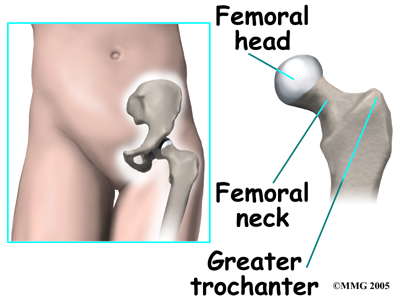
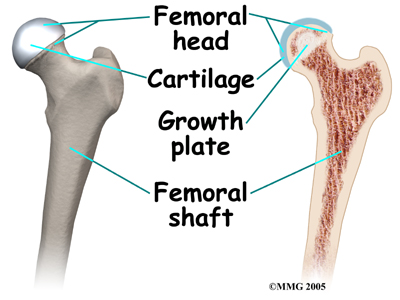
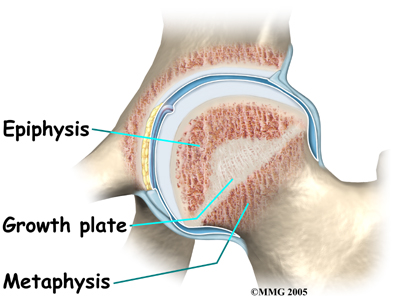
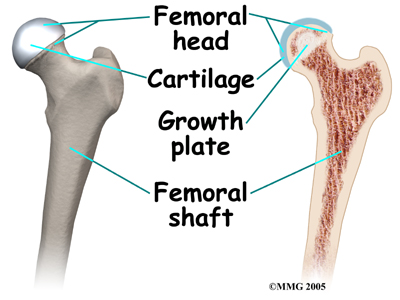
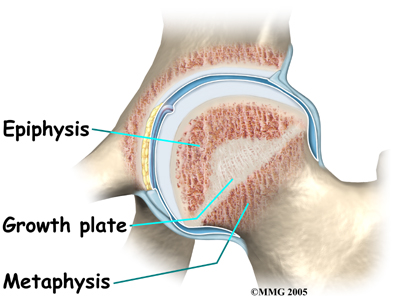
In the growing child, there are special structures at the end of most bones called growth plates. The growth plate is sandwiched between two special areas of the bone called the epiphysis and the metaphysis. The growth plate is made of a special type of cartilage that builds bone on top of the end of the metaphysis and lengthens the bone as we grow. In the hip joint, the femoral head is one of the epiphyses of the femur.
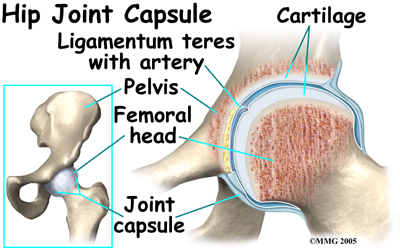
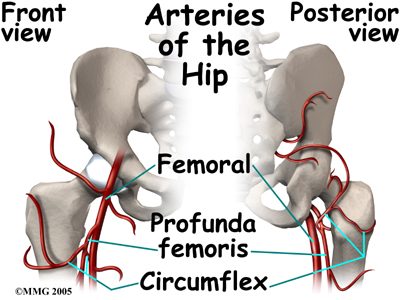
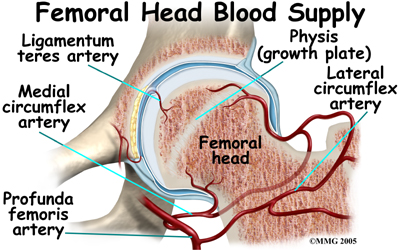
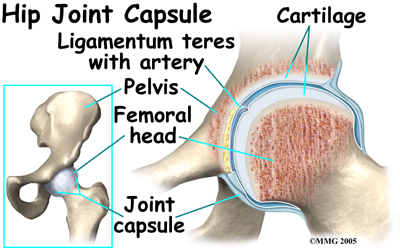
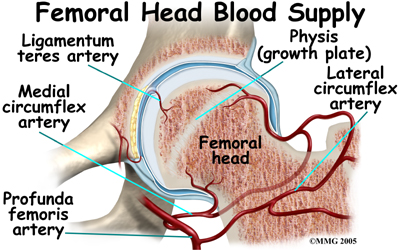
The capital femoral epiphysis is somewhat unique. It is one of the few epiphyses in the body that is inside the joint capsule. (The joint capsule is the tissue that surrounds the joint.) The blood vessels that go to the epiphysis run along the side of the femoral neck and are in danger of being torn or pinched off if something happens to the growth plate. This can result in a loss of the blood supply to the epiphysis.
Causes
How does this problem develop?
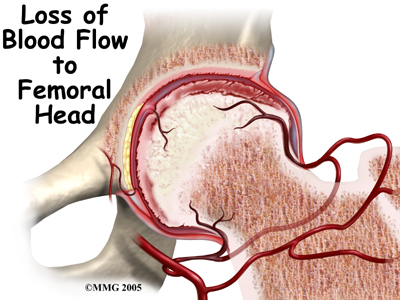
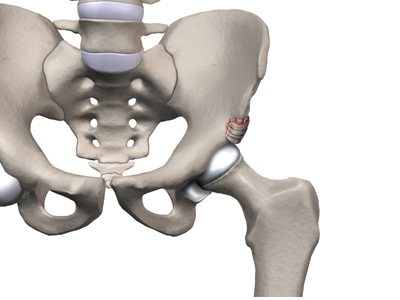
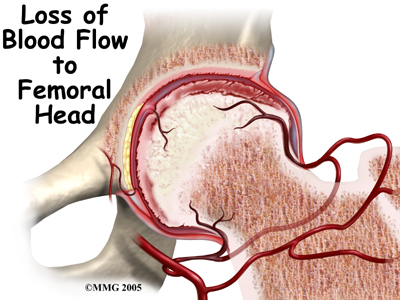
Perthes disease results when the blood supply to the capital femoral epiphysis is blocked. There are many theories about what causes this problem with the blood supply, yet none have been proven. There appears to be some relationship to nutrition as children who are malnourished are more likely to develop this condition.
 Children who have abnormal blood clotting (a condition called thrombophilia) may also have a higher risk of developing Perthes disease. These children have blood that clots easier and quicker than normal. This may lead to blood clotting that blocks the small arteries going to the femoral head. As a result of new evidence, the certainty of thrombophilia as a cause of Perthes is now under debate. This will remain an area of study until scientists clear up the significance of thrombophilia as a possible cause of Perthes.
Children who have abnormal blood clotting (a condition called thrombophilia) may also have a higher risk of developing Perthes disease. These children have blood that clots easier and quicker than normal. This may lead to blood clotting that blocks the small arteries going to the femoral head. As a result of new evidence, the certainty of thrombophilia as a cause of Perthes is now under debate. This will remain an area of study until scientists clear up the significance of thrombophilia as a possible cause of Perthes.
There is some new evidence that Perthes disease may be genetic as a result of a mutation (abnormal change) in the type II collagen (fibers that make up soft tissue structures). Previously there was no known increase in risk for children whose parent had Perthes disease as a child, but this belief may no longer be accurate.
Studies among Asian families who have many family members with this disease have been found with this mutation in the type II collagen gene. Scientists think that the mutation results in weakening of the hip joint cartilage that also affects the blood vessels within the cartilage.
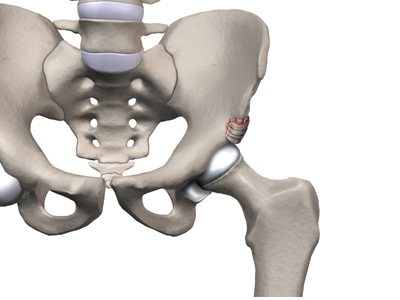
Whatever the true cause of ischemia (lack of blood to the area), the result is bone death (called necrosis) of the femoral head. Without a normal blood supply, the bone loses its strength and shape. The loss of bone density and softening of the head result in a femoral head that is misshaped. With the hip supporting the weight of the body, tiny microfractures in the soft, necrotic bone fail to heal. This is another reason why normal wear and tear results in a deformity.
Symptoms
What does this problem feel like?
Most children with Perthes disease develop discomfort in the hip and walk with a limp. Children will not usually complain of pain unless specifically asked. The most common way that the disease is discovered is when someone, usually a parent, notices the limp and consults a physician.
When the doctor examines the hip, the motion of the hip is abnormal and restricted. Turning the leg inward produces pain. This usually indicates that the hip is inflamed and may have inflammatory fluid (called an effusion) present in the hip joint.
Interestingly, problems in the hip sometimes do not cause pain in the hip itself. The knee is where the pain is felt. This can be confusing both to patients and physicians. In general, a child with knee pain (who has no clear-cut reason to have knee pain), or an abnormal gait, should be examined for possible Perthes disease. This usually includes X-rays of the hips to make sure that Perthes disease is not missed.
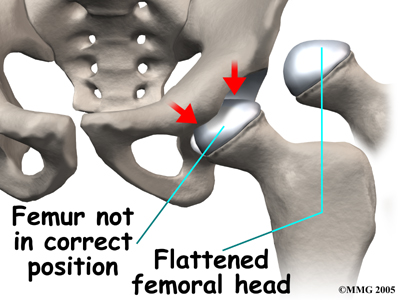 The main problem with Perthes disease is that it changes the structure of the hip joint. How much it affects the way the hip joint works depends on how much the hip joint is deformed. Muscle weakness and atrophy affecting the thigh and calf muscles may develop over time. The affected leg can shorten as a result of the changes in the hip. The result may be a significant leg length difference. Problems later in life are more likely the greater the deformity after the condition has healed.
The main problem with Perthes disease is that it changes the structure of the hip joint. How much it affects the way the hip joint works depends on how much the hip joint is deformed. Muscle weakness and atrophy affecting the thigh and calf muscles may develop over time. The affected leg can shorten as a result of the changes in the hip. The result may be a significant leg length difference. Problems later in life are more likely the greater the deformity after the condition has healed.
In general, the most common problem later in life is the development of arthritis in the hip joint. The type of arthritis that develops in the hip is osteoarthritis (also known as wear and tear arthritis). Just like a machine that is out of balance, the hip joint wears out and becomes painful.
Diagnosis
How do health care professionals identify the problem?
The history and physical examination are usually enough to make your health care professional highly suspicious about the diagnosis of Perthes disease. X-rays are usually necessary to confirm the diagnosis. It is usually not necessary to get an MRI scan to make the diagnosis, however, this test may be useful to determine whether the other hip is involved in the disease. A special MRI using a dye called gadolinium may help show changes in blood supply before anything shows up on an X-ray.
In planning treatment another test, called an arthrogram, may be required. In this test, dye is injected into the hip joint to outline the cartilage surface of the joint. Much of the child's hip joint is made up of cartilage. Cartilage does not usually show up on X-rays. The dye is necessary to see what the hip will actually look like when the cartilage turns to bone.
Treatment
What treatment options are available?
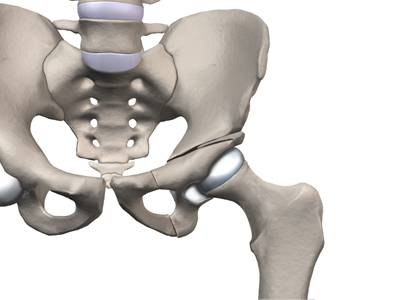
The primary goal of treatment for Perthes disease is to help the femoral head recover and grow to a normal shape. The closer to normal the femoral head is when growth stops, the better the hip will function in later life. The way that surgeons achieve this goal is using a concept called containment.
Containment is a simple concept. The femoral head can be molded as it heals. This is very similar to molding plastic. Plastic is poured into a mold and held there as it cools. It then holds the shape of the mold. The hip socket, or acetabulum, is not affected when the femoral head loses its blood supply. It can be used as a mold to shape the femoral head as it heals. The trick is that the femoral head must be held in the joint socket (acetabulum) as much as possible, however, it is better if the hip is allowed to move and is not held completely still in the joint socket. Joint motion is necessary for nutrition of the cartilage and for healthy growth of the joint.
All treatment options for Perthes disease try to position and hold the hip in the acetabulum as much as possible. This healing process can take several years.
Many children who are diagnosed with Perthes disease do not require any treatment except careful watching. When the condition is mild, the results of not doing anything are often as good as aggressive treatment. The majority of children who are treated for Perthes disease these days require only a program for maintaining a near-normal range of motion. This may include nighttime splinting, home traction, and physiotherapy (see below.) The surgeon will determine treatment based on the classification of the severity of the disease. The classification is determined by the X-ray findings.
Nonsurgical Treatment
Maintaining or regaining hip motion to as near to normal as possible, is critical to the successful treatment of Perthes disease. The disease causes inflammation in the joint. This leads to loss of motion and contracture (tightening) of the muscles surrounding the hip joint. Treating these problems to restore normal motion is necessary.
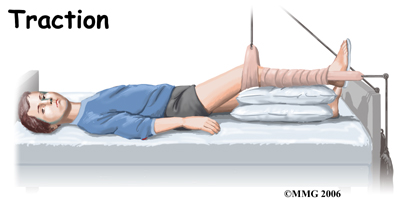
When lack of motion has become a problem, the child may be admitted to the hospital and placed in traction. Traction is used to give the joint some space and therefore quiet the inflammation. The rest for the joint while in traction also helps to settle the inflammation. Settling the inflammation usually takes about a week. Home traction may also be an option.
Anti-inflammatory medications may also be prescribed. In addition, antiresorptive agents may also be prescribed. These medications help to slow or block the resorption of bone and help decrease deformity. Studies are being done to fully test the effect of these medications in children with Perthes.
 Physiotherapy while in the hospital is used to restore the hip motion as the inflammation comes under control. A physiotherapist will visit your child in their room and assist them with some gentle hip rotation and abduction exercises (taking the leg out to the side.) These exercises will maintain and improve range of motion but will also assist in moving the fluid inside the hip joint, which assists with joint nutrition and is crucial to healing. They will also show you and your child how to continue the exercises independently once your child leaves the hospital if you will be using a home traction unit, and may prescribe further simple exercises that your child should do once they are no longer in traction. Your physiotherapist may even recommend that your child do some exercises in the pool to take advantage of the hydrostatic properties of the water to gain range of motion with less weight bearing impact.
Physiotherapy while in the hospital is used to restore the hip motion as the inflammation comes under control. A physiotherapist will visit your child in their room and assist them with some gentle hip rotation and abduction exercises (taking the leg out to the side.) These exercises will maintain and improve range of motion but will also assist in moving the fluid inside the hip joint, which assists with joint nutrition and is crucial to healing. They will also show you and your child how to continue the exercises independently once your child leaves the hospital if you will be using a home traction unit, and may prescribe further simple exercises that your child should do once they are no longer in traction. Your physiotherapist may even recommend that your child do some exercises in the pool to take advantage of the hydrostatic properties of the water to gain range of motion with less weight bearing impact.
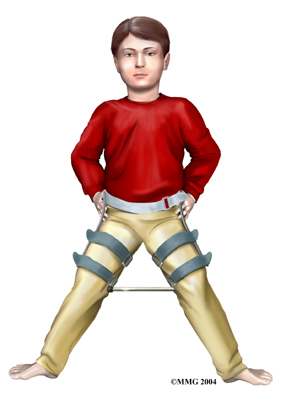
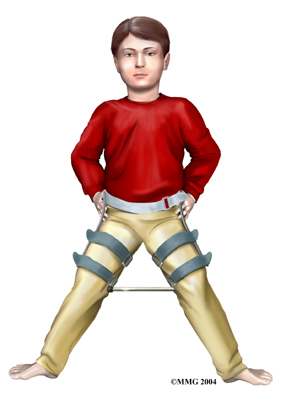
In the past, surgeons have tried to hold the hip in the best position where the femoral head was molded by the acetabulum using many different casts and braces. The most common way of doing this today is the Scottish Rite Orthosis. This brace fits around the waist and thighs and has hinges at the hip joints. The brace allows the child to walk and play while it holds the hip joint in the best position for containment. Your doctor may prescribe this for your child once they leave the hospital. Your physiotherapist will help your child learn to safely use crutches or a walker/frame if they are needed while in the brace.
Surgery
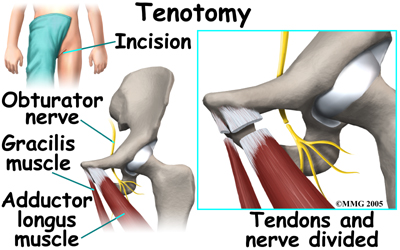
Sometimes, adequate motion cannot be regained with traction and physiotherapy alone, therefore in some cases, surgery will be required to obtain adequate containment. If the condition is longstanding, the muscles may have contracted or shrunk and cannot be stretched back out. To help restore motion, the surgeon may recommend a tenotomy of the contracted muscles. When a tenotomy is performed, the tendon of the muscle that is overly tight is cut and lengthened. This is a simple procedure that requires only a small incision. The tendon eventually scars down in the lengthened position, and no functional loss is noticeable.
 Surgical treatment for containment may be best in older children who are not compliant with brace treatment or where the psychological effects of wearing braces may outweigh the benefits. Surgical containment does not require long-term braces or casts. Once the procedure has been performed and the bones have healed, the child can pursue normal activities as tolerated.
Surgical treatment for containment may be best in older children who are not compliant with brace treatment or where the psychological effects of wearing braces may outweigh the benefits. Surgical containment does not require long-term braces or casts. Once the procedure has been performed and the bones have healed, the child can pursue normal activities as tolerated.
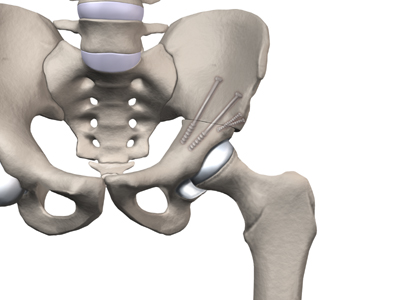
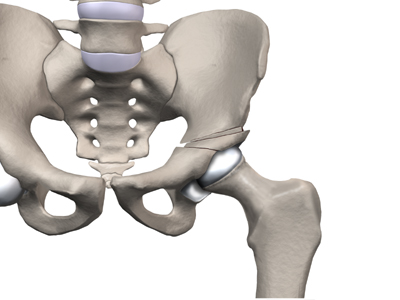
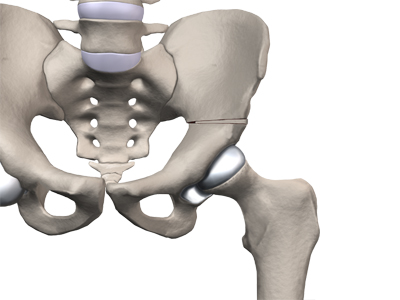
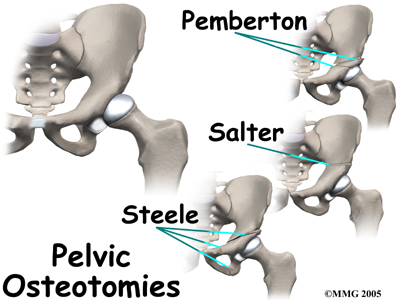
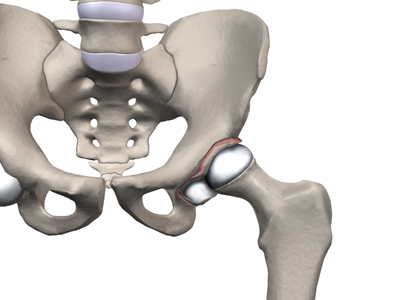
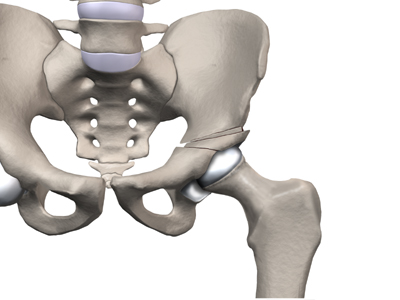
Surgical treatment for containment usually consists of procedures that realign the femur (thighbone), the acetabulum (hip socket), or both.



Realignment of the femur is called a femoral osteotomy. This procedure changes the angle of the femoral neck so that the femoral head points more towards the socket. To perform this procedure, an incision is made in the side of the thigh. The bone of the femur is cut and realigned in a new position. A large metal plate and screws are then inserted to hold the bones in the new position until the bone has healed. The plate and screws may need to be removed once the bone has healed.
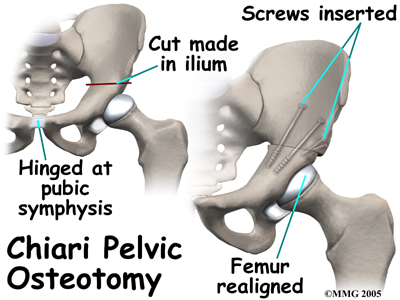
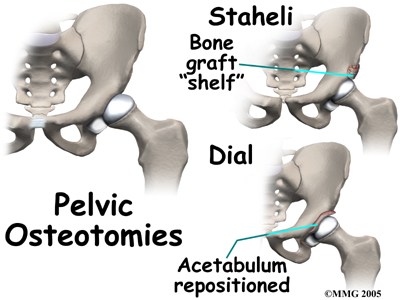
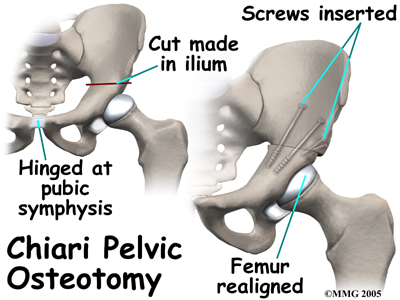
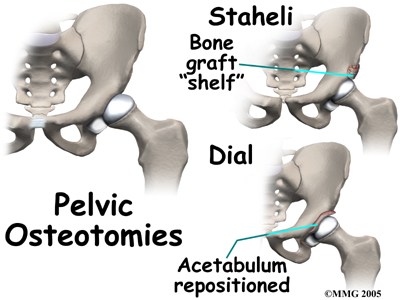
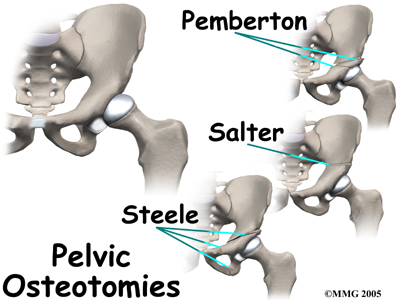
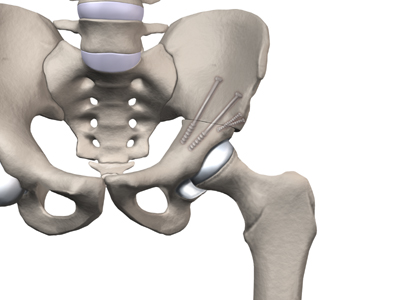
Realignment of the acetabulum is called a pelvic osteotomy. This procedure changes the angle of the acetabulum (socket) so that it better covers, or contains, the femoral head. To perform this procedure, an incision is made in the side of the buttock. The bone of the pelvis is cut and realigned in a new position. Large metal pins or screws are then inserted to hold the bones in the new position until the bone has healed. The pins usually must be removed once the bone has healed.
If there is a serious structural change in the anatomy of the hip, there may need to be further surgery to restore the alignment closer to normal. This is usually not considered until growth stops. As a child grows, there will be some remodeling that occurs in the hip joint. This may improve the situation such that further surgery is unnecessary.
In severe cases, both femoral osteotomy and pelvic osteotomy may be combined to obtain even more containment.
Osteotomy Types
Rehabilitation
What should I expect from treatment?
Following surgery for Perthes disease, physiotherapy treatment at In Balance Physiotherapy is very useful in returning your child to their pre-injury activity level as quickly as possible. Physiotherapy can also assist in avoiding other compensatory problems in the back or lower limb in the future as well as to restore and regain any strength and range of motion deficits that have developed as a result of the disease up to this point.
Rehabilitation at In Balance Physiotherapy can begin as soon as your child’s surgeon recommends it. Each surgeon will set his or her own specific restrictions based on the child’s individual severity of injury, the surgical procedure used, personal experience, and whether the hip is healing as expected.
If your child is still suffering from any residual pain from the surgical procedure when they come to In Balance Physiotherapy for their initial appointment, your physiotherapist may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing the pain. If your child is walking with a walker/frame or crutches, your physiotherapist will ensure your child is using the crutches safely and appropriately and that they are abiding by any weight bearing restrictions set by their surgeon. Your physiotherapist will also ensure that your child can safely use the crutches on stairs.
We generally recommend that until it is possible to walk without a significant limp, either a walker or one or two crutches continue to be used. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to continue on crutches until near normal walking can be achieved. Your physiotherapist will give advice regarding the appropriate time for your child to be walking without any support at all, although with young children, the ongoing use of a walking aid, even if recommended, can be difficult as they tend to discard them once they can get around without them. Once your child is no longer using any walking aid your physiotherapist will assist with normal gait re-education.
The next part of our treatment at In Balance Physiotherapy will focus on normalizing any deficits that may have developed in the range of motion and strength of your child’s lower limbs. Your physiotherapist may assist in stretching your child’s limb or lower back while at the clinic and, if necessary, will ‘mobilize’ the joints of your child. This hands-on technique encourages the stiff joints to move gradually into their normal range of motion. In addition to the hands-on treatment in the clinic we will also prescribe a series of stretching exercises that we will encourage your child to do as part of a regular home exercise program. We will especially focus on maintaining or gaining range of motion in the surgical hip.
Similarly to the range of motion deficits, strength deficits will also be addressed. Strength building exercises particularly for the hip will be taught in the clinic and added to your child’s home program. For older children we may incorporate items such as Theraband or light weights into the exercises to provide additional resistance for the limb. If your child is still young your physiotherapist will explicitly explain how you can work with your child to complete the stretching and strengthening exercises. We will provide ideas for ways that you can incorporate the exercises into your child’s daily play routine.
The final part of our physiotherapy treatment at In Balance Physiotherapy will be ensuring that your child’s coordination and balance have returned to normal after their surgery. Following even a short period of walking with crutches or a period where your child is walking abnormally due to pain, your child’s normal balance, coordination, and proprioception (the ability to know where your body is without looking at it) can decline in function. Exercises, which may include balancing on one foot, jumping, and quick agility movements will be encouraged at an appropriate time in line with the surgeon’s restrictions.
Fortunately, gaining lost range of motion, strength, and coordination after surgery for Perthes disease happens quickly. You will notice improvements in your child’s function and gait even after just a few treatments with your physiotherapist at In Balance Physiotherapy. If, however, your child’s post-surgical therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to confirm that the hip is tolerating the rehabilitation well and ensure that there are no post-surgical complications that may be impeding your child’s recovery. Generally your child’s surgeon will follow-up quite regularly anyways to monitor symptoms, check on hip mobility, and to make sure that the condition is not deteriorating, so appropriate progression of rehabilitation is easily monitored as well. The surgeon will also take X-rays during their follow-up visits to determine the healing of the femoral head.
Despite optimal surgical and post-surgical care, patients with Perthes disease are always at higher risk of developing osteoarthritis of the hip. The end result is that most patients with Perthes disease will require an artificial hip at some point in the future. Most patients do not develop problems for 40 years or more. How soon patients have problems with their hip is directly related to how much deformity remains once the condition heals. In general, the more round the femoral hip is at that time of complete healing, the longer the hip will stay free of pain.
Portions of this document copyright MMG, LLC
In Balance Physiotherapy provides services for physiotherapy in Toronto.
 Perthes disease is a condition that affects the hip in children between the ages of four and eight. The condition is also referred to as Legg-Calve-Perthes disease in honor of the three physicians who each separately described the disease. In this condition, the blood supply to the growth center of the hip (the capital femoral epiphysis) is disturbed, causing the bone in this area to die. The blood supply eventually returns, and the bone heals. How the bone heals determines what problems the condition will cause in later life. Perthes disease may affect both hips. In fact, 10 to 12 percent of the time the condition is bilateral (meaning that it affects both hips). This condition can lead to serious problems in the hip joint later in life.
Perthes disease is a condition that affects the hip in children between the ages of four and eight. The condition is also referred to as Legg-Calve-Perthes disease in honor of the three physicians who each separately described the disease. In this condition, the blood supply to the growth center of the hip (the capital femoral epiphysis) is disturbed, causing the bone in this area to die. The blood supply eventually returns, and the bone heals. How the bone heals determines what problems the condition will cause in later life. Perthes disease may affect both hips. In fact, 10 to 12 percent of the time the condition is bilateral (meaning that it affects both hips). This condition can lead to serious problems in the hip joint later in life.








 Children who have abnormal blood clotting (a condition called thrombophilia) may also have a higher risk of developing Perthes disease. These children have blood that clots easier and quicker than normal. This may lead to blood clotting that blocks the small arteries going to the femoral head. As a result of new evidence, the certainty of thrombophilia as a cause of Perthes is now under debate. This will remain an area of study until scientists clear up the significance of thrombophilia as a possible cause of Perthes.
Children who have abnormal blood clotting (a condition called thrombophilia) may also have a higher risk of developing Perthes disease. These children have blood that clots easier and quicker than normal. This may lead to blood clotting that blocks the small arteries going to the femoral head. As a result of new evidence, the certainty of thrombophilia as a cause of Perthes is now under debate. This will remain an area of study until scientists clear up the significance of thrombophilia as a possible cause of Perthes.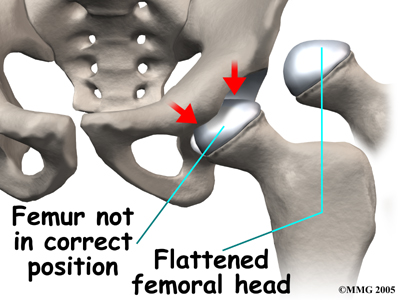 The main problem with Perthes disease is that it changes the structure of the hip joint. How much it affects the way the hip joint works depends on how much the hip joint is deformed. Muscle weakness and atrophy affecting the thigh and calf muscles may develop over time. The affected leg can shorten as a result of the changes in the hip. The result may be a significant leg length difference. Problems later in life are more likely the greater the deformity after the condition has healed.
The main problem with Perthes disease is that it changes the structure of the hip joint. How much it affects the way the hip joint works depends on how much the hip joint is deformed. Muscle weakness and atrophy affecting the thigh and calf muscles may develop over time. The affected leg can shorten as a result of the changes in the hip. The result may be a significant leg length difference. Problems later in life are more likely the greater the deformity after the condition has healed.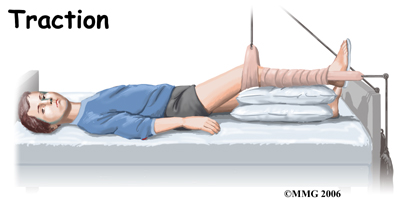
 Physiotherapy while in the hospital is used to restore the hip motion as the inflammation comes under control. A physiotherapist will visit your child in their room and assist them with some gentle hip rotation and abduction exercises (taking the leg out to the side.) These exercises will maintain and improve range of motion but will also assist in moving the fluid inside the hip joint, which assists with joint nutrition and is crucial to healing. They will also show you and your child how to continue the exercises independently once your child leaves the hospital if you will be using a home traction unit, and may prescribe further simple exercises that your child should do once they are no longer in traction. Your physiotherapist may even recommend that your child do some exercises in the pool to take advantage of the hydrostatic properties of the water to gain range of motion with less weight bearing impact.
Physiotherapy while in the hospital is used to restore the hip motion as the inflammation comes under control. A physiotherapist will visit your child in their room and assist them with some gentle hip rotation and abduction exercises (taking the leg out to the side.) These exercises will maintain and improve range of motion but will also assist in moving the fluid inside the hip joint, which assists with joint nutrition and is crucial to healing. They will also show you and your child how to continue the exercises independently once your child leaves the hospital if you will be using a home traction unit, and may prescribe further simple exercises that your child should do once they are no longer in traction. Your physiotherapist may even recommend that your child do some exercises in the pool to take advantage of the hydrostatic properties of the water to gain range of motion with less weight bearing impact.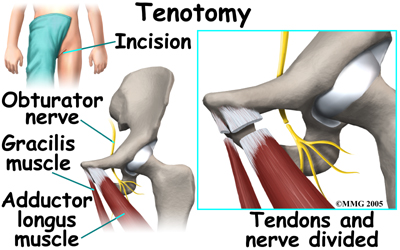 Surgical treatment for containment may be best in older children who are not compliant with brace treatment or where the psychological effects of wearing braces may outweigh the benefits. Surgical containment does not require long-term braces or casts. Once the procedure has been performed and the bones have healed, the child can pursue normal activities as tolerated.
Surgical treatment for containment may be best in older children who are not compliant with brace treatment or where the psychological effects of wearing braces may outweigh the benefits. Surgical containment does not require long-term braces or casts. Once the procedure has been performed and the bones have healed, the child can pursue normal activities as tolerated.